Ya Gotta Have Heart; I Almost Didn’t.
To anyone searching this site for new material the last couple of weeks, my apologies. But I have a pretty good excuse. I had unscheduled quadruple bypass surgery last Tuesday and returned home from the hospital a couple of days ago. I am lucky.
Chest pain
Because this site appeals to many baby boomers who are in those "susceptible" years, I will offer a few notes and lessons learned here about the last two weeks of my life, and about how the preceding years may have contributed to the intense pain in my chest I felt while in a recliner chair, totally at rest watching a movie, on Thursday January 26, a day that seemed, until the chest pain, not unlike any other. In fact, I had ventured out of the house for a drive to a board meeting at a local non-profit at lunchtime. I ate little at lunch -- soup, a piece of coffee cake and a bottle of water – hadn’t expended much energy and felt just fine. Dinner was slightly less ordinary. (See below.)
But that evening, the pain I felt in my chest was like nothing I had ever encountered. I know indigestion, and this was no indigestion. It was like two strong tug-of-war teams fighting hard, with the center of the rope at my chest. I had set up my "man cave" in the basement only a week earlier, and by the time I had made it up the stairs to tell my wife Connie of the pain, I was winded beyond relation to the number of stairs.
Please make it the anchovies
 I still wanted to believe this was a unique form of indigestion, especially since my half of the pizza we shared two hours earlier included anchovies, a food I eat rarely (and these were not the best-tasting anchovies). But after a few Tums and no relief, I thought we might be in heart attack territory.
I still wanted to believe this was a unique form of indigestion, especially since my half of the pizza we shared two hours earlier included anchovies, a food I eat rarely (and these were not the best-tasting anchovies). But after a few Tums and no relief, I thought we might be in heart attack territory.
Lesson: Chest pain does not necessarily mean heart attack, as the doctors told me later. In my case, the pain was a signal of blockage in at least one of my arteries. (See more below.)
Lesson: Blood pressure readings tell you little about the state of your heart at any one moment. My wife and I took my blood pressure readings before the Tums (170/95) and after (138/90); the doctors later indicated neither was predictive of anything.
The closest emergency room
 The pain was so bad that I really had little choice other than to ask Connie to drive me to the UCONN (University of Connecticut) Health Center in Farmington, CT, just 12 minutes from our home. I would have preferred admission to Hartford Hospital, where I had an earlier surgery and a few other trips to the hospital's emergency room for me and my wife, but UCONN was half the distance.
The pain was so bad that I really had little choice other than to ask Connie to drive me to the UCONN (University of Connecticut) Health Center in Farmington, CT, just 12 minutes from our home. I would have preferred admission to Hartford Hospital, where I had an earlier surgery and a few other trips to the hospital's emergency room for me and my wife, but UCONN was half the distance.
Lesson: Even if you think you can ride out the pain, or it isn't intense enough to check into, resist the urge to wait. Either call 911 -- I certainly had that option -- or if the hospital is fairly close, have someone drive you. Right away.
I thought the admissions process in the hospital emergency room at 9 pm was a bit casual for a patient complaining of chest pains. (No other patients were in the waiting room or behind me in line.) I was not given an aspirin immediately, one way to address a possible heart attack, and since I was already in the medical center's computer system, I thought there were too many questions at that point. But the intake person was friendly, showed concern and ushered me into a room within five minutes or so. And frankly, I wasn't feeling any worse while I sat waiting.
Lesson: Things don't always move in a hospital at a pace that seems reasonable. You're the patient (customer); you have every right to demand an explanation, if not action, when you believe you might be at risk. Many hospitals will send a representative to see you toward the end of your stay to ask your opinion about their services. That's nice, but altogether too late.
Not a heart attack, but...
 I'll proceed quickly through the diagnostic stuff in the ER. I had none of the customary signs of a classic heart attack; no sweating, no pains shooting up and down arms, no nausea. But the intense chest pains I described to the doctors and the fact that I am diabetic and take pharmaceuticals for high blood pressure and cholesterol gave them cause for concern about my heart. The only way they could conclusively decide about what was at the source of my pain was with an angiogram, an invasive procedure in which dye is shot through an artery, makes its way to your heart and renders beautifully contrasted photos of arteries and veins.
I'll proceed quickly through the diagnostic stuff in the ER. I had none of the customary signs of a classic heart attack; no sweating, no pains shooting up and down arms, no nausea. But the intense chest pains I described to the doctors and the fact that I am diabetic and take pharmaceuticals for high blood pressure and cholesterol gave them cause for concern about my heart. The only way they could conclusively decide about what was at the source of my pain was with an angiogram, an invasive procedure in which dye is shot through an artery, makes its way to your heart and renders beautifully contrasted photos of arteries and veins.
Lesson: I thought a stress test was supposed to determine whether one had heart problems. Not so, said the doctors. I had a stress test -- intense walking/running on a treadmill while monitored by nurses and a doctor -- three years earlier in preparation for another surgery. But the stress test shows how strong your heart is, not necessarily whether there is any arterial blockage. And it comes with risks, especially if you are having chest pains. I opted for the angiogram, which was performed the morning after admission. They administered an anesthesia that permitted me to be awake, but only faintly so; if I had experienced pain, they wanted to hear me moan about it. But there was zero pain involved and the 45-minute procedure seemed to take 5 minutes.
...not a pretty picture
The pictures showed 90% blockage in three arteries. I was introduced to a surgeon, Dr. Daniel Fusco, who patiently explained the status of my heart and offered a Hobson's choice of two options. (Hobson is the guy who offers you a choice that is in the category of take it or leave it.) Choice one was triple bypass surgery, which carries an extremely slight risk of stroke or death. Choice two was to place stents in the affected arteries, basically providing a pathway for blood around the plaque-ridden areas. The problem with the second choice was that the size of one of the arteries was large enough that failure within a year or two was likely; but doctors do not typically open up a patient to do a single bypass. After asking all the questions I could, I was confident bypass surgery was the right approach.
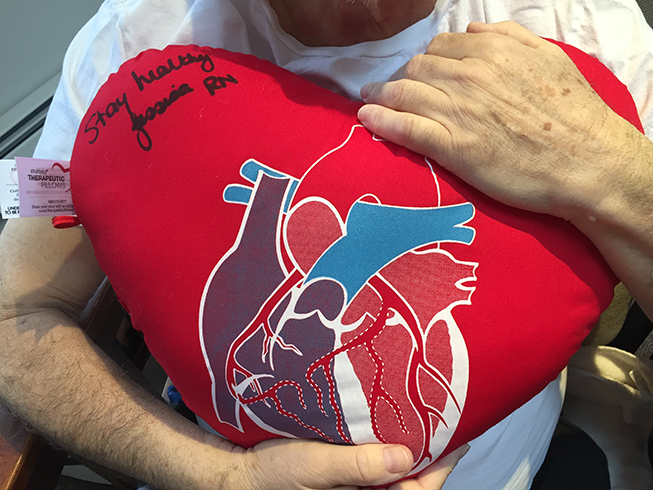 The hospital's cardiology nurses give you a cute going away present, a pillow in the shape of a heart. Some of them sign it. But the pillow has a practical use as well; when you cough after the operation, clutching it to your chest helps relieve some of the pain. Some.
The hospital's cardiology nurses give you a cute going away present, a pillow in the shape of a heart. Some of them sign it. But the pillow has a practical use as well; when you cough after the operation, clutching it to your chest helps relieve some of the pain. Some.Lesson: You might logically ask yourself about how I "chose" my doctor. At this point, it was almost like being at Walmart shopping for a TV and the salesperson says, "Trust me, Sharp is better than Samsung." Trust you? I don't even know you. When I learned Dr. Fusco was "assigned" as my surgeon, but before I met with him, I did some quick Internet research. He had performed thousands of bypass surgeries, had a great track record and everyone praised his bedside manner. I certainly could have phoned friends quickly for any recommendations, but those would have been hearsay. I liked Dr. Fusco when I met him, we talked about family as well as hearts, and I decided that intuition and gut instinct, which rarely fail me, was the best guidance in a situation that needed attending to quickly. It was also fundamental that Connie liked him as well. (After the fact, I learned that Dr. Fusco was a mechanical engineer by training and occupation for some years before deciding to become a doctor; having worked during my career with engineers, I know they sweat the details as much as any professional does. And Dr. Fusco has also performed multiple heart transplants; they typically demand up to 12 hours of rapt attention, and my surgery was to be 3 hours.)
After the angiogram, surgery was scheduled for the following Tuesday. I felt well enough to return home for the intervening few days but the doctors insisted I stay for the extra prep necessary in the run-up to such a serious operation. It is not fun to be hooked up to a drip -- Heperin, to make sure I developed no clots before surgery -- and to have intravenous tubes that were only used occasionally...or to have monitors constantly beeping nearby...or to have your vital signs checked every four hours. A hospital is the last place you ever want to go for a good night's sleep. But the security of knowing I had immediate help within steps if something should go wrong soothed my anxiety about being away from home.
Lesson: Listen to your doctors about length of stay in the hospital. Trust me, they want you out of there as quickly as possible to free up beds and deal with one fewer patient. If they say you should remain there for an extra day or two, believe it.
Tackling another blocked artery
The surgery itself was, of course, a non-event for me. That is, I slept through all of it and the total four hours passed as if it were just four minutes. In the hour before the operation, the attending nurse had trouble finding a receptive artery in my arm for the IV, but she was more upset than I (but not that upset). I had no weird dreams while under anesthesia, and I came out of the fog gradually but pretty quickly. When I awoke, my cheery-faced wife and daughter were at my bedside in ICU, indicating to me that something pretty good had happened (that I was still alive). At some point, whether compelled by relief or drugs, I mimicked the Schwarzenegger line and gasped, “He’s baaack!” My daughter liked that. I learned later, when I was a bit more awake, that a fourth blocked artery that was hidden from view (or just didn't accept any dye during the angiogram) was bypassed as well. Dr. Fusco had visited my wife and daughter in the surgery waiting room and told them the operation had gone "perfectly." In the succeeding days, I felt as if that was not hyperbole; mindful that I was on some light painkilling drugs, I still felt wonderful, good enough to chip and putt. And toward the end of my four-day post-op stay, I was feeling especially good. But that was the painkillers talking and the fact that the incision area and cracked ribs hadn’t begun to heal, which is painful.
 I am about 7 weeks away from my first round of golf which likely will take place at Pawleys Plantation Country Club. Chipping and putting will probably precede that by two weeks.
I am about 7 weeks away from my first round of golf which likely will take place at Pawleys Plantation Country Club. Chipping and putting will probably precede that by two weeks.
Lesson: Do not be deceived if you find yourself in the same situation, feeling better than you expect. This is major surgery, you have taken a body check from the equivalent of a 240-pound hockey defenseman (or worse), and my first days at home have demonstrated that there will be pain (although nothing major and only in the incision area and part of the leg near the knee where they removed an artery to use as bypass material). I found I was allergic to the adhesive on the EKG patches they put on your chest, but a combination of hydrocortisone cream -- though applied nowhere near any incisions -- and Benadryl has helped.
Diet, exercise and the other lifestyle stuff
 I understand there are changes I need to make to my lifestyle in order to keep more trouble with my heart at bay. Before this incident and surgery, I thought my heart was healthy, with no real family history, that the stress test I passed a couple of years ago was a sign of a strong heart and that my eating habits which, if not exactly heart-healthy, were not a threat. Certainly, I will be ratcheting back on the sodium intake, and the red meat I indulged every 10 days or so may become once per month, and less fatty at that. I like tofu, and there are a bunch of things one can do with tofu, although it will never be mistaken on my palate for a one-pound Porterhouse.
I understand there are changes I need to make to my lifestyle in order to keep more trouble with my heart at bay. Before this incident and surgery, I thought my heart was healthy, with no real family history, that the stress test I passed a couple of years ago was a sign of a strong heart and that my eating habits which, if not exactly heart-healthy, were not a threat. Certainly, I will be ratcheting back on the sodium intake, and the red meat I indulged every 10 days or so may become once per month, and less fatty at that. I like tofu, and there are a bunch of things one can do with tofu, although it will never be mistaken on my palate for a one-pound Porterhouse.
For me, though, it is mostly about activity, or the lack thereof. I am a 68-year old who opts for a golf cart even at times the course is flat and I am feeling up to a good walk. That will certainly change this year. I am also going to force myself onto a treadmill at least a few days a week. There is no excuse not to; through AARP membership, those of us over the age of 65 can obtain a "Silver Sneakers" card which provides free admission on an unlimited basis at many fitness centers. Mine is just 15 minutes away. (You can check if your own health plan includes Silver Sneakers membership here.)
Life is short; live it while you can
One other lifestyle change I intend to make starting this summer: Limiting excuses for travel and exploration. There is always some convenient excuse for my wife and me not to travel: Get the house ready for sale in a few years, community or personal activities near our home in Connecticut, or as my beloved Brooklyn Dodgers used to say before they won their first World Series, "Wait 'til next year." No more; I just booked a Caribbean vacation for Connie, me, our grown children and their significant others this summer. Of course, a few nice golf courses are nearby..
If anyone has any questions, please let me know and I will be pleased to set up a dialogue. This was not an experience for the faint of heart (pun intended), and if I can help anyone feel more comfortable about it, that is the least I can do. Contact me by clicking here. If you are reading this, that means you either hung in there while I was gone, or you are a new reader. In either case, I am deeply appreciative.